Streamlining Healthcare Data Exchange with HL7 Interface Engines
Keyur Patel
September 12, 2025
18 min
HL7 integration helps in proper communication between healthcare systems and devices, thus cutting out the time-consuming process of manual entry of data and the occurrence of errors. It can also assist in lowering the expenses of the medical facilities and patients since there will be less likelihood of repeat tests or procedures. health level seven integration can enhance patient services such as scheduling, reminders, and other appointment-related services and ease the interaction between patients and healthcare providers.
Why Health Industry Need an HL7 Interface Engine?
Health level 7 Interface Engine depends on sharing information across different systems and sites, so these are precisely where HL7 technologies must be integrated. It creates cross-vendor translation and interconnects the most isolated silos of data, ensuring the seamless flow of critical medical information.
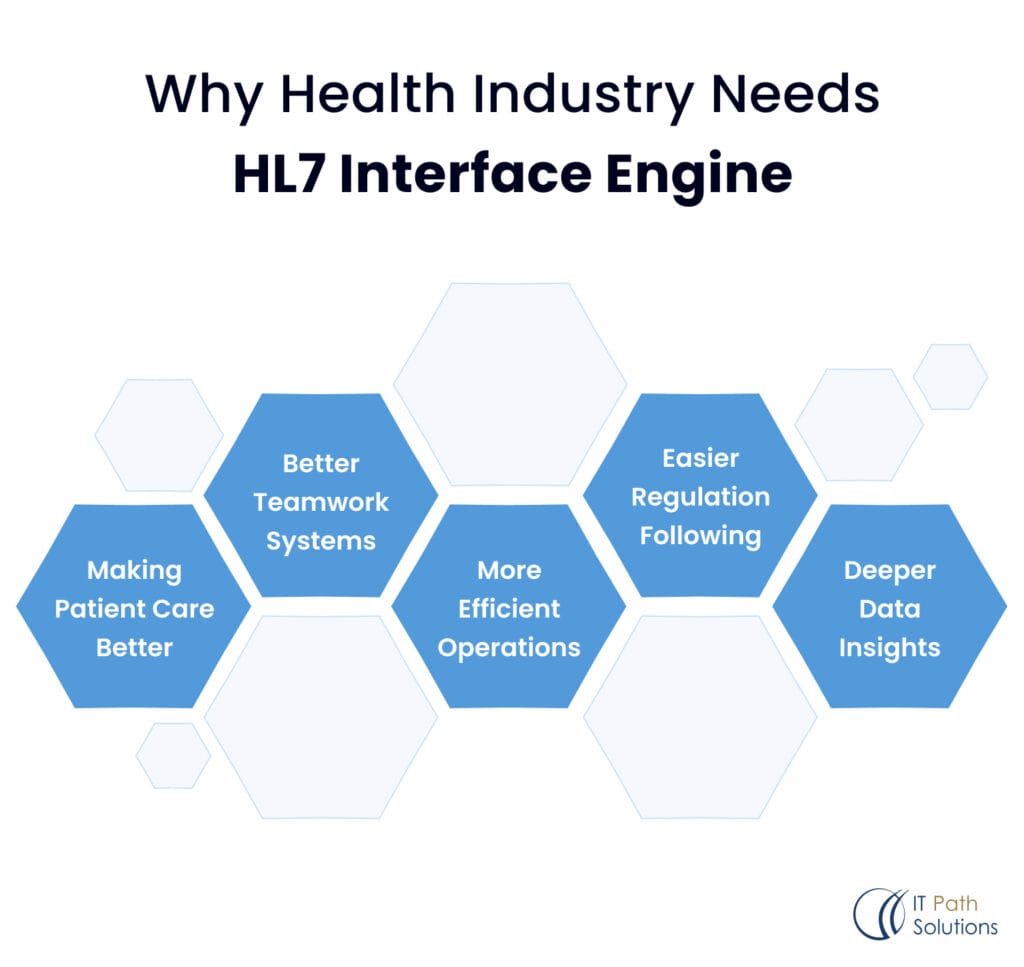
Enhancing Patient Care
The need for the exchange of accurate information should be emphasized especially regarding issues to do with patients. An HL7 interface engine also guarantees that all the critical data, including the patient’s history, allergies, and the list of medications they take, are always shared across systems. This minimizes the chances of making mistakes and improves the quality of the patients’ healthcare.
Improved Team Dynamics
Think of every department in a hospital using different software that can’t “talk” to the other pieces of mobile application software and seems seriously out of sync. In comes HL7 integration, managing to get them all to work like a single unit; the data flows back and forth from one department to another, without any hitches.
Enhancing Workflow Productivity
An HL7 messaging engine significantly reduces the time required to integrate various healthcare systems. Traditional methods of system integration often involve lengthy and complex processes of coding, testing, and deploying custom interfaces for each system connection. With an HL7 connectivity engine, the process becomes more streamlined and standardized, allowing for quicker setup and modification of interfaces.
Compliance with Regulations
The healthcare sector has to abide by some stringent rules regarding data privacy, much like HIPAA. Usually, keeping compliance is an administrative nightmare, but with HL7 integration, it might be a breeze. Proper care of sensitive information is taken through encryption, access control, and auditing, among others, in the best way so the standard will adequately cover you on all legal bases. Then, adherence to the regulations is just a breeze.
Enhanced Data Analytics
With HL7 integration, all patient medical data can be standardized and speak the same, clear language, allowing for robust analysis. This improves accuracy in identifying care quality issues, optimizes treatment plans with detailed outcome data, and enables predictive AI modeling. These revolutionary insights transform healthcare delivery.
Now let’s move on to the next topic Process Behind HL7 Integration in Healthcare
The Process Behind HL7 Integration in Healthcare
HL7 integration in healthcare involves mapping and translating data between different systems using standard HL7 messages, ensuring seamless communication and interoperability across diverse healthcare IT platforms.
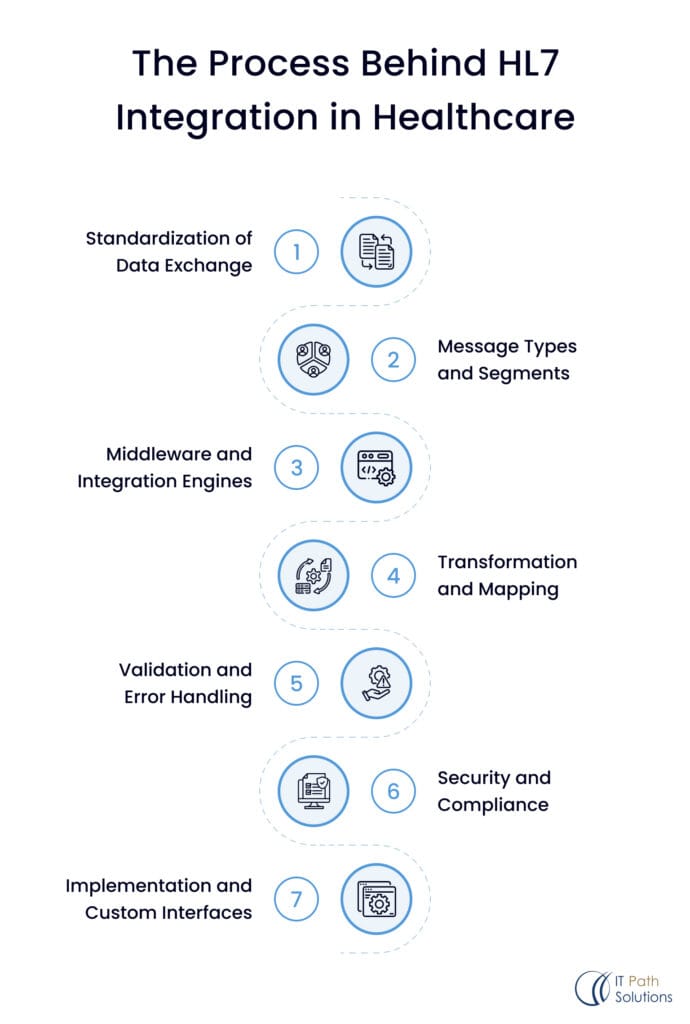
1. Standardization of Data Exchange
HL7 defines the structure and format of the messages that are exchanged between systems. These messages include various types of healthcare information exchange, such as patient records, lab results, billing information, and clinical observations. The most commonly used standards are HL7 Version 2. x, HL7 Version 3, and FHIR (Fast Healthcare Interoperability Resources, not a fancy hair treatment).
2. Message Types and Segments
HL7 messages are composed of segments, each containing specific types of data. For example, a message might include segments for patient information, order details, and lab results. Each segment has a specific format and set of fields defined by HL7 standards, ensuring consistent data representation.
3. Middleware and Integration Engines
This is where the real magic happens. Middleware tools, such as Mirth Connect, Rhapsody, and Corepoint, manage the flow of HL7 messages between different systems. They can route, transform, and translate messages to ensure they are correctly interpreted by the receiving system. Middleware also handles various protocols and communication methods, such as TCP/IP, HTTP, and web services.
4. Transformation and Mapping
Despite the HL7 standards, some systems still like to be unique little snowflakes with their way of representing data. Transformation and mapping processes act as the diplomats, converting one format to another so any miscommunications are averted.
5. Validation and Error Handling
Validation tools check HL7 messages are legit and follow the protocol. If they find an error, some systems will politely decline the message, while others might try an on-the-fly fix.
6. Security and Compliance
Healthcare data is sensitive stuff, so HL7 integration has to lock it down with encryption, authentication, and full compliance with fun regulations like HIPAA.
7. Implementation and Custom Interfaces
Some systems require custom HL7 integration with additional requirements. Integration experts have to develop these special interfaces through coding and configs to keep those systems integrated with the rest.
Some of the systems need to have Custom HL7 integration with the extra requirement
So it is crucial for healthcare data exchange. It ensures our medical records move smoothly between systems, like a vital flow of information
How Does HL7 (Health Level 7) Integration Engine Work
The integration engine is another key element in modern infrastructures for healthcare IT, as it allows for data exchange and communication across several systems. With the thousands of interfaces built around the HL7 messaging standard, this engine enables integration and interoperability among different applications and platforms, making it a central interface engine.
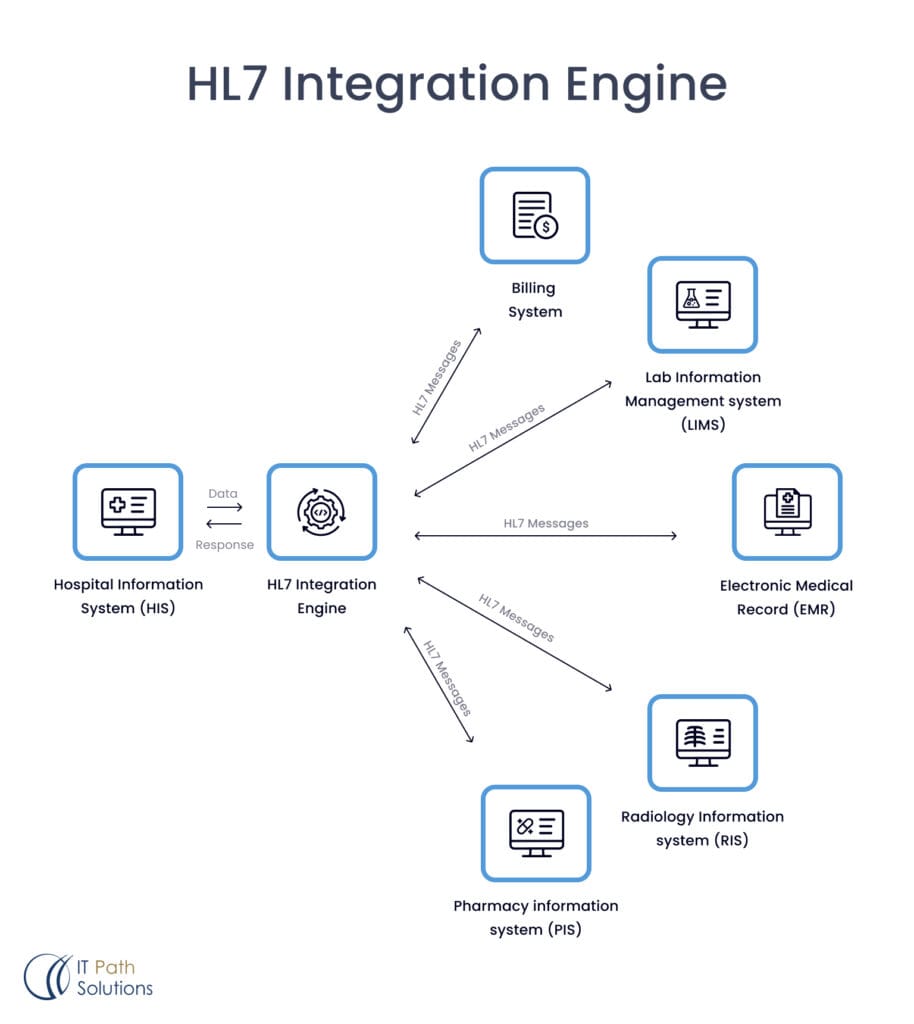
Hospital Information System — HIS
The central repository for various types of patient data—including demographics, medical history, appointments, and admissions—is an HIS. If the HIS needs to share data with other systems, it can put the bits of information in the HL7 format, ensuring that it is capable of working with the other parts of the healthcare realm.
HL7 Integration Engine
That is where things get interesting. The integration engine receives the neatly formatted HL7 data payloads from the HIS and acts as a translator, taking this data and translating it to specific formats so it becomes compliant with the various receiving systems. It manages data transformations, mappings, and routing to make sure the right information gets to the right place in the right form.
An integration engine is essential to allow the free flow of information between different healthcare IT systems, including:
Billing System:
HL7 interface engine connects to clinical and administrative systems that typically store the financial records of the organization and provide the billing platform with the most up-to-date insurance, patient balances, and service charges. union ensures that the bills are correctly produced with all relevant codes and coverage details, facilitating smooth reimbursement processes.
Laboratory Information Management System (LIMS) :
The integration engine manages the bi-model data flow between the LIMS and other systems. The diagnostic test requests, cultures, and critical laboratory results are automatically shared with the Electronic Medical Record (EMR) and other systems to serve the current diagnostic information to the medical staff. On the other side, new lab requests are routed from the EMR or other ordering systems toward the LIMS, so the workflow is smoother.
An Electronic Medical Record (EMR) :
Patient charts where all the clinical documentation, medication-based charts, imaging data, lab results, and other related reports from all the clinic daily visits/consultations are consolidated into the centralized repository, which is either scanned or written into the system.
Doctor on Demand with HL7 integration provides a streamlined telehealth experience by ensuring that patient data is consistently and accurately shared between the telemedicine platform and other healthcare systems.
The glue of this data is the integration engine that acts to connect this raw data and create a complete, evolving digital health record for healthcare providers to consume and update. It is an EMR interface engine that allows for the data integration of several systems on the market into your EMR.
Radiology Information System (RIS) :
X-rays, CT scans, and MRI images are obligatory for accurate patient care to make a diagnosis of a disease. This visual data exchange is shared between the RIS and the EMR (as well as other systems that need imaging results) via a layer we call the integration engine. The seamless integration allows for fast review and collaboration by physicians, ensuring that diagnostic information is easily accessible.
Pharmacy Information System (PIS)
Due to the importance of prescription management in patient care, the HL7 integration engine is very useful in managing information flow between the PIS and other systems. Thus, the integration engine that connects the PIS to the EMR and other clinical management platforms ensures the availability of an up-to-date list of medications while forwarding new prescriptions. Telemedicine app development with HL7 integration enables seamless exchange of clinical information between different healthcare systems. It enhances healthcare accessibility, especially for those in remote or underserved areas.
This integration enables healthcare providers to renew and alter prescriptions to make sure that these are properly taken and filled to enhance patient care.
Aside from these core systems, the HL7 healthcare interface engine can integrate HL7 messages with other healthcare applications like patient self-service interfaces, clinical decision support tools, and population health management systems. As the new version of HL7 FHIR (Fast Healthcare Interoperability Resources) comes into the market, the integration engine is being developed to support HL7 FHIR integration to facilitate data sharing via web services and APIs.
Many organizations outsource HL7 integration to specialized services that offer cloud-based solutions for data modeling, transformation, and message routing. Some companies prefer self-hosted systems, using various HL7 integration software from different providers. These tools enable the creation of custom interfaces, helping design, develop, test, and deploy integrations. Features like visual mapping tools and monitoring dashboards cater to specific integration needs.
Use Cases of HL7 Integration
Let’s look at some concrete scenarios where HL7 interface integration becomes utterly indispensable:
Electronic Medical Records (EMR) for New Patients
Isn’t it just great when you don’t have to go through the whole set of questions that new patients are asked to answer again? In HL7, EHR records were transferred without much of a problem. It was a simple data exchange, and your new doctor is already prepared with your information.
Information Exchange Between Hospitals
Whatever the scenario an emergency admission or a specialist referral – HL7 is the solution to the records backlog that occurs when providers are unable to share information. In an API-based data-sharing model, your health information is wirelessly transmitted between providers, improving your care.
Information Exchange with Regulators
The transfer of Electronic Health Records (EHR) was smooth and easy. This ensured that your new doctor received all your medical information and was well-prepared for your visit.
Shift Management
Scheduling employees is always a challenge, especially in the medical field where the shifts are on a round-the-clock basis and certain ratios need to be observed in terms of staffing.
When HL7 links employee skills data, patient loads, time-off requests, and other factors into smart scheduling software, you get the best staff balances to reduce overwork and enhance care.
Patient Services
More patients want to schedule appointments, check test results, and refill prescriptions on their phones. For these services to be secure, strong data protection is needed, and that’s where the latest HL7 standard, FHIR, helps.
Process Automation
It always comes in handy for every healthcare institution to take a break from all the meaningless paperwork that is a drain on resources. HL7 has very specific data formatting, which means that you can connect systems and automate processes; orders, labs, patients, etc, will all be directed to the required systems. No hands need apply.
API-Oriented HL7 Integration Platform
API-oriented HL7 integration means the integration of HL7 with various healthcare systems with the help of APIs. This approach has been found to make the flow of data easier as compared to the earlier methods of transferring data.
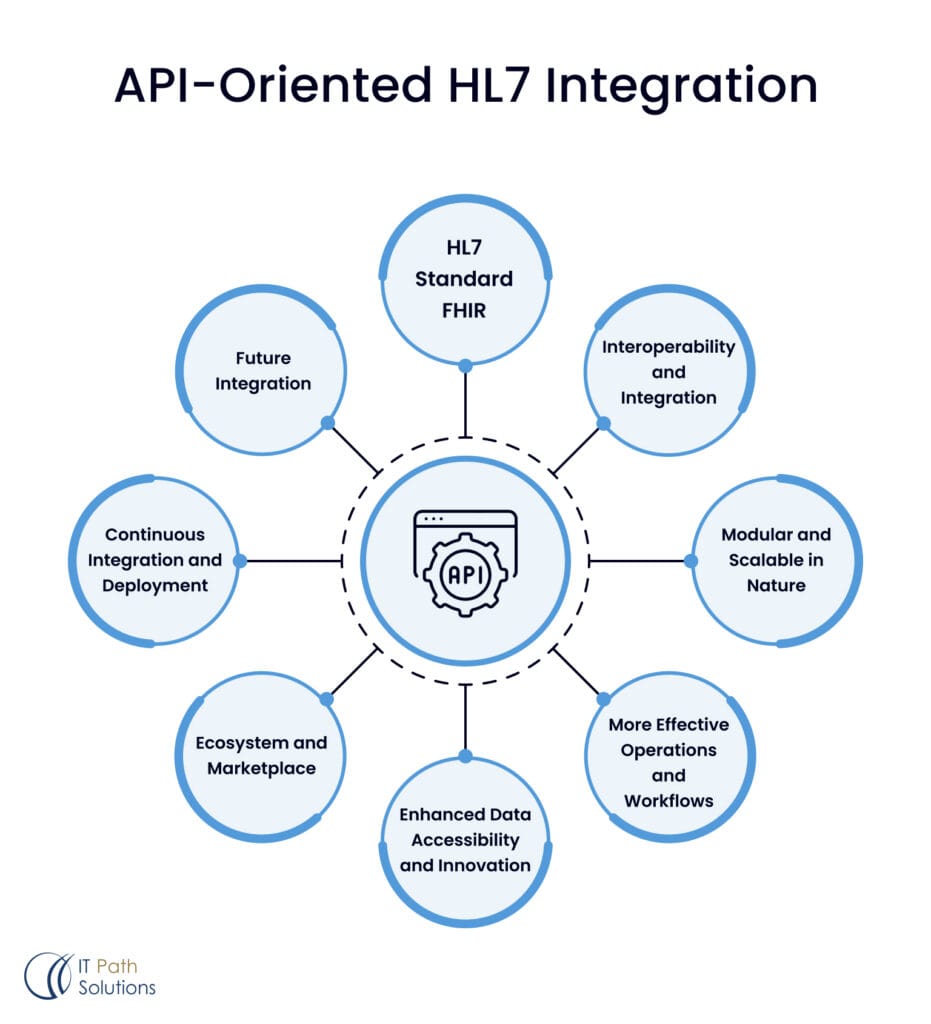
1. HL7 Integration Modernization with Restful Apis
HL7 messaging protocols particularly HL7 version 2. x, are rather old and can be inconvenient, they are like attempting to construct a high-rise building out of childish blocks. Point-to-point interfaces and message-based communication can be dirty and intricate. APIs are far more contemporary and effective like a knight in shining armour.
2. HL7 Standard FHIR
HL7 FHIR, the final entry on this list of APIs, is well-suited for healthcare API integration. It leverages RESTful APIs and uses modern, lightweight data formats like JSON and XML. These are the latest and most advanced technologies in the field.
3. Interoperability and Integration
APIs help different healthcare systems, devices, and apps work together smoothly by providing clear interfaces for data and functions. This allows for real-time data exchange and coordination. In the world of data, it’s all about teamwork, with everyone collaborating to make sure everything works well together.
4. Modular and Scalable in Nature
Consider outsourcing HL7 integration to specialized services that provide cloud-based solutions for data flow modeling, transformation, and message routing. Alternatively, some organizations choose self-hosted systems, integrating HL7 software from various providers. These tools help create custom interfaces for designing, developing, testing, and deploying integrations, with features like visual mapping tools and monitoring dashboards to meet specific needs.
5. More Effective Operations and Workflows
APIs have brought about the efficiency we’ve needed, providing direct access to application data and functions. This bypasses complex intermediate systems, speeding up data access and improving decision-making and workflow for healthcare providers. It’s a straightforward solution that simplifies processes without any unnecessary complications.
6. Enhanced Data Accessibility and Innovation
He noted that the policy promotes innovation by permitting the regulated use of health data. This includes applications like healthcare mobile app development(mHealth) and digital health monitoring, and various analytics tools, setting the stage for new and exciting trends in healthcare.
7. Ecosystem and Marketplace
This would establish a new market and environment for the sales of health applications. It enables care organizations to collaborate and interface with one thousand third-party applications through APIs. It is active for users to build new services and applications as it is a community of users.
8. Continuous Integration and Deployment
Robust APIs can help support the Agile methods and CI/CD practices by embracing the best practices of the modern SDLC and architecture. It makes it possible to attempt to implement changes to the system as often as one can and ensure that they do it in time to meet the new and ever-changing needs of the business. It is similar to having a large group of rather awake developers on the clock who are maintaining your systems and making them as lively and beautiful as possible.
9. Future Integration
The API approach will one day result in new standards for connecting healthcare systems. APIs will offer a stable base of new technologies and integration approaches that will appear in the future. But, it’s as if we have got a peek into the future of health IT, but no wires, no magic.
HL7 integration is right on course to an API-oriented approach so is already halfway there. So, I suppose it is high time to get rid of this rather, shall we say, archaic approach, didn’t you? Healthcare IT systems as well as your sanity will be grateful to you for this.
Complexities and Hurdles in Facilitating Seamless HL7 Data Exchange
However, various complexities and hurdles exist in facilitating the seamless HL7 data exchange to improve the quality of healthcare delivery systems. This paper seeks to elucidate some of these challenges encountered in the process of implementing HL7 data integration system.
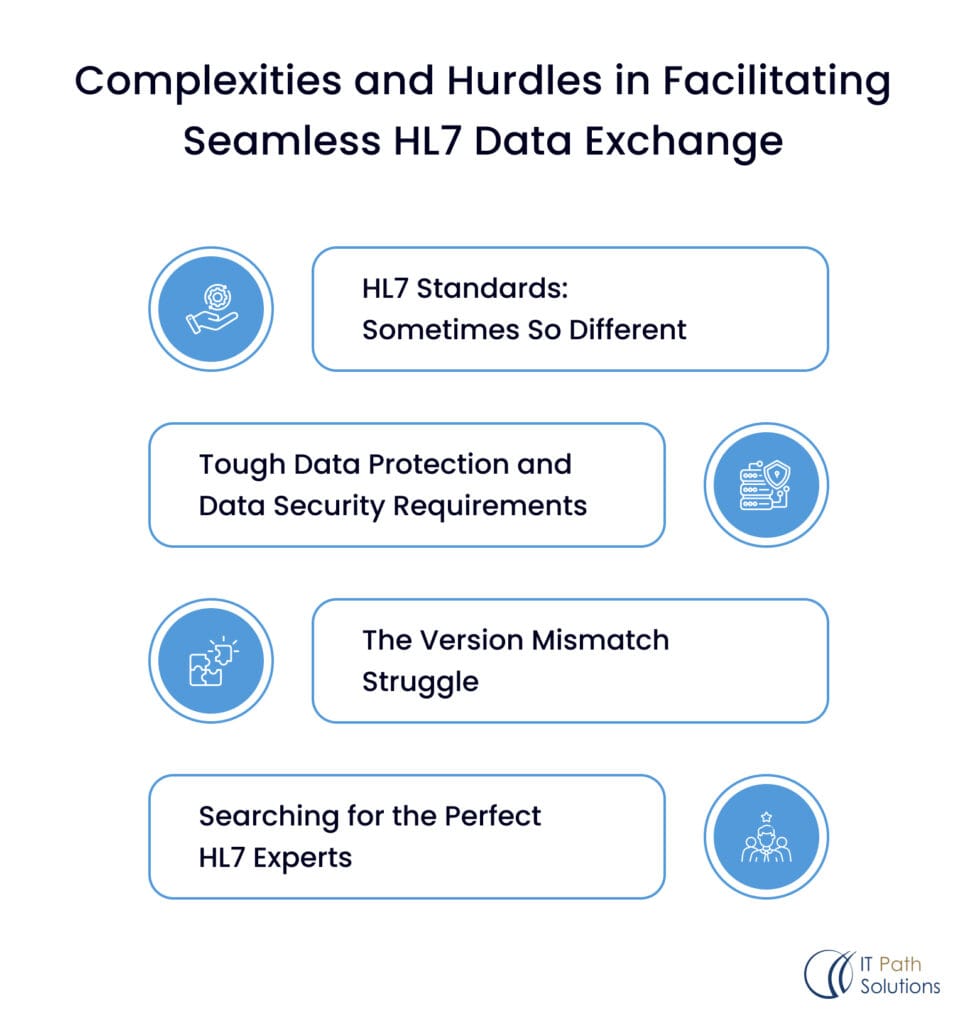
HL7 Standards: Sometimes So Different
In an ideal world, the HL7 standard would guarantee the accuracy of translated data interchange between medical caregivers across language barriers. The reality? Everyone, in essence, involuntarily created their regional accents over time. Ultimately, integrating all of those micro differences and all those special cases is a huge mapping problem, which is essentially understanding everybody’s home cultured language. This is further complicated by the fact that there are still older versions of HL7 in use within aging Healthcare Infrastructure.
Tough Data Protection and Data Security Requirements
This one’s pretty self-explanatory: It is one of the most sensitive types of data that can be found in existence. It is your private information that you are sharing with people, thus there can be no compromises when it comes to safety. New system integration means there is a new and likely vulnerable entry point that requires impenetrable security, auditing and control, and full HIPAA-compliant measures. There is no room for compromises where one mistake could lead to mass destruction.
The Version Mismatch Struggle
The HL7 world is, therefore, a vast one, with new versions and standards being brought into the market even as older ones remain relevant in production systems. It is quite complicated, and that is why converting data between different incompatible versions is a true hack. It is managing an outrageous number of schemas and relationships while transitioning to, say, FHIR without losing or altering any of the data.
Searching for the Perfect HL7 Experts: A Continuous Process
Being that the specialized knowledge required for designing and maintaining such systems is almost always scarce and constantly in high demand. HL7 integration experts, who know the ins and outs of the system, the differences in standards, and security requirements, are rare gems. It is a challenging and very expensive task to identify and acquire talent that is uniquely suited to an organization’s IT team. There is no way that any team can approach this game without preparation.
So yeah, standardization of system integration, which is to say that systems must work together without issue, remains the objective, and yet the landscape is filled with some rather rough around the edges examples of integration challenges – from standardization fragmentation to the rigor of data management. However, avoiding the barriers is not an option as Healthcare organizations must achieve the full potential of their digital transformation investments.
The HL7 interoperability engine technology suite
Consequently, the HL7 integration tech stack includes Programming languages such as Java, C#, and Python, messaging standards, including HL7, FHIR, and DICOM protocols, TCP/IP and web services, databases like Oracle and PostgreSQL, integration frameworks including Apache Camel and Mule ESB, docker and Kubernetes for containerization, cloud services like AWS and Azure, and monitoring, security, testing too.
This set of stacks ensures the effective integration of healthcare systems and the utilization of reliable as well as industry-standard-compliant structures for data exchange.
| Tech | Description |
| Angular | TypeScript-fueled web app development |
| React | Building ultra-responsive UIs |
| Node.js | JavaScript runtime for server-side heroics |
| Vue.js | The Swiss Army Knife of progressive web frameworks |
| .NET | Microsoft’s main squeeze for web domination |
| MySQL | Open-source database muscle |
| SQL Server | Microsoft’s enterprise-grade data |
Costs and Maintenance Demands of Proprietary HL7 Integration Implementations
| Cost and Demand | Description |
| Vendor Lock-in | Difficulty and high costs associated with switching to alternative solutions or migrating to different platforms due to vendor lock-in. |
| Customization and Consulting Fees | Additional fees for customizations, configurations, and consulting services from the vendor to tailor the solution to specific needs. |
| Ongoing Maintenance and Support Costs | Expensive ongoing maintenance and support contracts for software updates, bug fixes, and technical support from the vendor. |
| Upgrade and Migration Challenges | Complex and costly processes for upgrading to newer versions or migrating to different platforms often require downtime, data migration efforts, and additional consulting services. |
| Limited Flexibility and Extensibility | Lack of flexibility and extensibility to adapt to evolving healthcare standards, regulations, or changing organizational needs, potentially leading to costly workarounds or additional third-party tools. |
| Staffing and Training Requirements | Costs associated with specialized training and certifications for in-house staff to work with the proprietary solution. |
| Integration with Third-Party Systems | Challenges and additional costs for integrating proprietary solutions with third-party systems or applications, potentially requiring custom integrations or purchasing additional modules or connectors. |
| Limited Transparency and Control | Lack of transparency in the underlying architecture, code, and data structures, limits an organization’s ability to fully understand and control the integration processes. |
| Scalability Limitations | Potential scalability challenges as healthcare organizations grow and data volumes increase, requiring costly upgrades or replacements to accommodate increasing demands. |
Conclusion
Modern healthcare relies on data sharing via HL7 integration, making it essential for efficient, high-quality care. Robust HL7 solutions tackle issues like inconsistent data practices and security gaps, helping break down barriers and improve care. With the right tools and expertise, organizations can achieve seamless data exchange and better outcomes.

Keyur Patel
Co-Founder
Keyur Patel is the director at IT Path Solutions, where he helps businesses develop scalable applications. With his extensive experience and visionary approach, he leads the team to create futuristic solutions. Keyur Patel has exceptional leadership skills and technical expertise in Node.js, .Net, React.js, AI/ML, and PHP frameworks. His dedication to driving digital transformation makes him an invaluable asset to the company.
Related Blog Posts

AI Healthcare Chatbot Development: Benefits, Use Cases, HIPAA Compliance, Challenges & How to Build One
A worried new mother sits awake at 2 a.m., startled by an unfamiliar cough from her infant. Instead of panicking or waiting until morning, she opens a HIPAA-compliant AI healthcare chatbot on her phone. She describes the symptoms, and within seconds, receives clear, trustworthy guidance. The chatbot reassures her, provides next steps, and even offers… AI Healthcare Chatbot Development: Benefits, Use Cases, HIPAA Compliance, Challenges & How to Build One

Medical Tourism In The Digital Age: How Technology And Apps Are Transforming Patient Care
A traveler books a flight for surgery abroad, then realizes the most challenging part is not the flight. It is comparing hospitals, reading outcomes, moving records, and staying connected during recovery. What if a trusted platform coordinated every step, from virtual consultations to post-care follow-ups, with price clarity and real-time support? That is the promise… Medical Tourism In The Digital Age: How Technology And Apps Are Transforming Patient Care
Develop App Like Firstline Benefits: A Complete Guide
The Firstline Benefits app has revolutionized how users access and manage their health and wellness benefits. By offering a seamless, user-friendly platform, Firstline Benefits has set a new standard in healthcare technology. If you’re looking to develop an app like Firstline Benefits, this guide will take you through every aspect—from key features to the tech… Develop App Like Firstline Benefits: A Complete Guide