Modernizing Legacy Systems in Healthcare: A Complete Guide
Keyur Patel
September 12, 2025
17 min
Legacy Systems in Healthcare
The shift from obsolete technology to innovative technologies is more important than ever. Organizations in the healthcare sector are dealing with the big issues that arise from the use of outdated systems to integrate them into the modern environment. This blog aims to present a detailed overview of the healthcare legacy systems, their effects on the patient, and ways to achieve the right modernization.
Healthcare legacy systems are defined as old software and hardware that are still being employed in healthcare organizations although better technologies exist. These systems were designed several years ago, but they continue to be the backbone of the functioning of numerous companies. They are still in use because of the challenges and expenses that come with replacing them with more efficient modern ones.
It is rather shocking to note that many medical organizations continue to use such systems, especially when there are better and more advanced systems in the market. A large number of hospitals and clinics use old clinical trial software that was created during the period between 1980 and 1990s, on outdated computers. These legacy medical technology solutions include EHR systems, billing systems, and medical imaging systems among others.
Types of legacy systems in healthcare
Different types of legacy systems are common in healthcare organizations and each of them is used for different purposes but has its issues. Let’s explore the most common types.
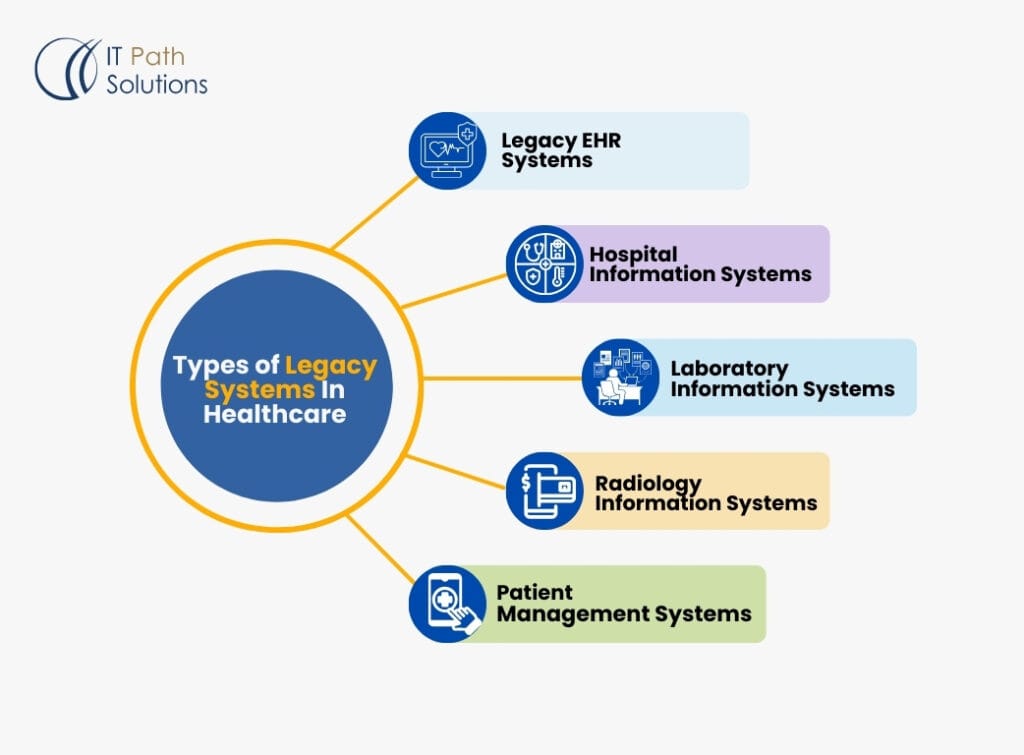
Legacy EHR Systems:
These are old systems used in the management of patient’s medical information through electronic data capture. Although those initial systems were revolutionary when implemented, many traditional EHR systems today suffer from interoperability issues, ease of use, and incorporation of current healthcare trends.
Hospital Information Systems (HIS):
Legacy HIS is used to handle several processes of hospitals such as registration, scheduling, and billing among others. Some of the older systems like Doctor on Demand may not be as adaptable as newer systems to changes in the delivery of healthcare and related regulations.
Laboratory Information Systems (LIS):
These systems are used in managing laboratory activities such as ordering tests, reporting results, and quality assurance. Legacy LIS may have difficulty in adopting new testing methodologies or interfacing with new healthcare devices.
Radiology Information Systems (RIS):
Legacy RIS coordinates the processes of organizing radiological imaging such as scheduling, image archiving, and reporting. Some of the older systems may have difficulties in dealing with the large data volumes characteristic of today’s imaging procedures or in interfacing with Picture Archiving and Communication Systems.
Patient Management Systems:
These systems deal with patients’ identification data, schedules, and payment details. Some previous PMS may not have functions for patient participation or face challenges with interoperability with other health systems.
Billing and Claims Processing Systems:
Old billing systems are likely to have issues with meeting the current and complex requirements of the healthcare billing process hence leading to inefficiency and loss of revenue.
All of these legacy systems contain problems in the current healthcare setting, such as security issues, and ineffective work and data flow. Exploring the effects and issues of these systems, it is easy to understand why modernization is not only advantageous but crucial for healthcare organizations that aim to deliver the best patient care in contemporary society.
The Impact of Legacy Systems on Healthcare Workflows
The continued use of healthcare legacy systems influences multiple aspects of medical practice.
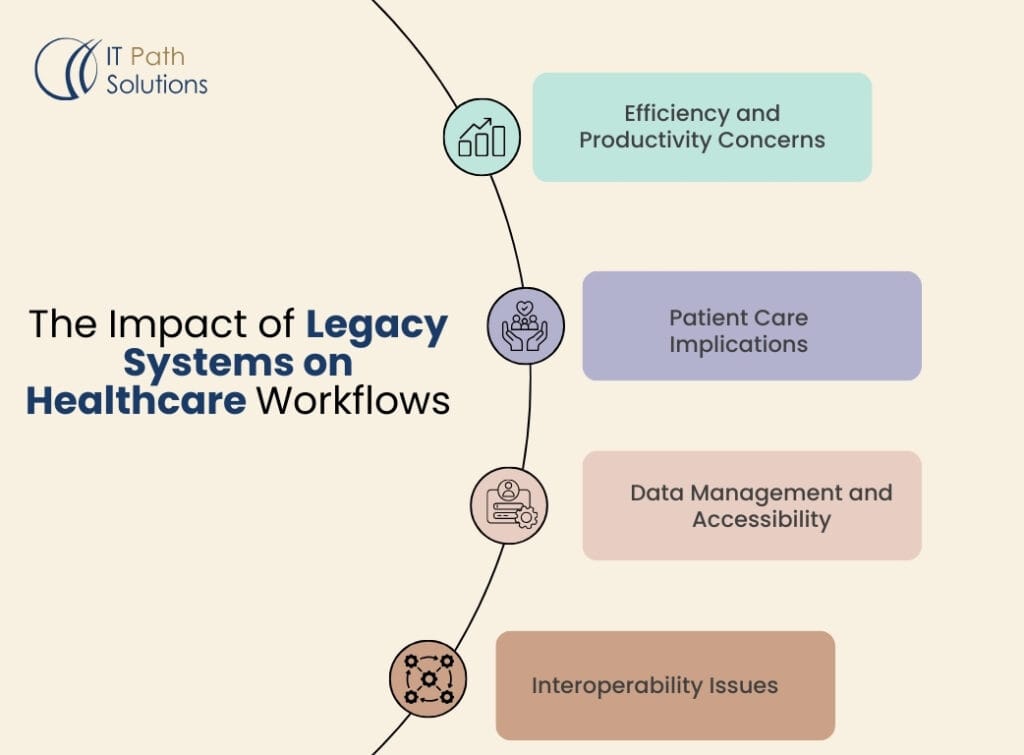
Efficiency and productivity concerns:
Old interfaces and slow processing slow down the performance of the staff. Many healthcare workers lose a significant amount of time dealing with inefficient processes, which limits the time spent on patients. For instance, a legacy EHR system can take many clicks and screen transitions simply to enter patient demographics into the record, which would slow the entire consultation.
Patient care implications:
Older hospital systems may not have features that are required for EBM and for making effective decisions. This can result in late diagnosis, treatment, and patient care management hence posing a threat to the health of patients. For instance, an old LIS may not be compatible with new diagnostic equipment, which could slow down the delivery of vital test results.
Data management and accessibility challenges:
Older systems are also characterized by problems with data integration and real-time data access. This limitation leads to the fact that patient records can be scattered, and a holistic picture of the patient’s status can be hardly obtained by the healthcare providers. An old generation of Radiology Information systems, for example, might not manage large imaging files well, which would slow down diagnosis.
Interoperability issues:
Some of the older medical technology solutions were developed with no consideration of integration and data sharing between systems or even healthcare facilities. This results in duplication of tests, wrong prescription of drugs, and areas of care being missed out on completely.
Key Challenges of Legacy Systems in Healthcare
In this context, healthcare organizations are presented with a myriad of challenges when it comes to working with legacy systems.
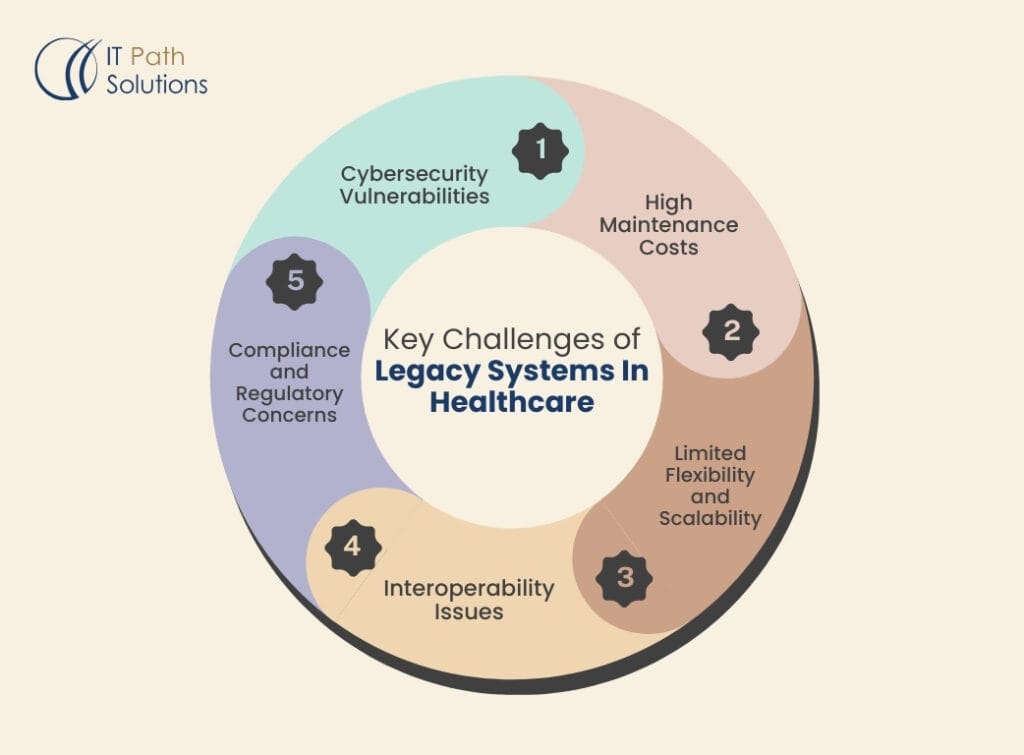
Cybersecurity vulnerabilities:
Old systems are also more vulnerable to attacks since they are not as updated as frequently as the newer systems. These vulnerabilities are quite dangerous as healthcare data security is now a very important issue hence threatening the privacy of patients and the integrity of the organizations. Some legacy systems may not have the current standard encryption or may not be capable of receiving security patches.
High maintenance costs: Maintenance
Legacy hospital systems become progressively costly as time goes by. Due to the vendors’ gradual withdrawal of support for outdated technologies, healthcare organizations may have to invest a lot of money to support such systems. This could mean having to recruit specialized staff or buying expensive and outmoded parts for computer equipment.
Limited flexibility and scalability:
The old systems can hardly cope with the new demands in the sphere of healthcare. They do not always adapt to new medical procedures, new technologies, or increasing patient base. For instance, a legacy Patient Management System may not support telehealth schedules or interact with patient portals.
Interoperability issues:
The older systems may not be compatible with the new technologies resulting in the creation of data silos and thus, inadequate comprehensive patient care. Such lack of compatibility may result in data duplication where the same information is entered into both systems, thus the risk of making mistakes is high.
Compliance and regulatory concerns:
Meeting current standards like HIPAA compliance can be challenging with outdated systems. As regulations evolve, legacy systems may fall short of required security and privacy measures, putting healthcare organizations at risk of non-compliance penalties.
Outdated user interfaces:
The interfaces of legacy systems are usually not user-friendly, and this causes users to become irritated and more prone to making mistakes. This can result in resistance to change by the users and the creation of substandard processes that would compromise the data integrity and overall efficiency of the system.
Managing Existing Legacy Systems: Best Practices
While planning for modernization, healthcare organizations must effectively manage their existing legacy systems: While planning for modernization, healthcare organizations must effectively manage their existing legacy systems:
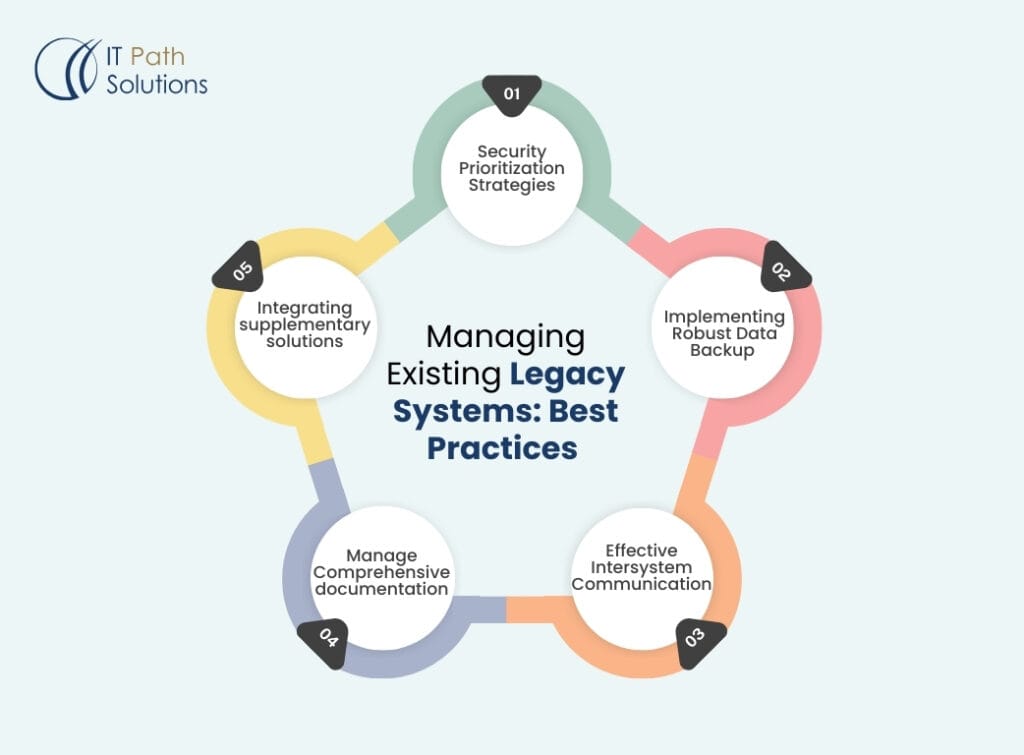
Security prioritization strategies:
Ensure that the weak systems are protected by sound security measures. This may include other firewalls, encryption techniques, and even security checks that may be conducted from time to time. In cases where the legacy systems cannot be replaced at the earliest, it is advisable to disconnect them from the main network to reduce vulnerability.
Implementing robust data backup and recovery plans:
It must guarantee the data’s consistency and accessibility when failures occur in the system. This means that data should be backed up regularly and the backup/recovery plan should be tested every once in a while. This is even more important for systems such as legacy EHRs where data loss could be catastrophic to the management of patients.
Establishing effective inter system communication:
Middleware solutions should be used to enhance communication between old and new architectures. This is because it can assist in excluding the gap between the old and new technologies hence improving the flow of data and minimizing data entry.
Maintaining comprehensive system documentation:
Ensure that you document the various aspects of the system in terms of architecture and other processes that are in place. It is advantageous for the documentation of troubleshooting and in case of further modernization of the system. It is particularly relevant to bespoke old-style applications that were developed by platform creators who may be out of work today.
Integrating supplementary solutions:
Integrate applications to extend the capabilities of the previous generation system. This can keep the existing systems productive while planning for a more radical transformation of the systems. For instance, a current reporting tool can be linked to an old Laboratory Information System to enhance data analysis functions.
Recognizing the Need for Modernization
The timing of upgrading or replacing old systems is very important in any organization. Signs that indicate the need for modernizing legacy healthcare systems include
Increasing maintenance costs:
When the cost of maintaining the existing systems becomes more than the cost of replacing those systems, then it is high time to go for modernization.
Frequent system downtimes:
The effectiveness of legacy systems means that if these are experiencing regular failures or minor performance problems, then the quality of patient care and organizational efficiency will also be affected.
Inability to meet regulatory requirements:
It also increases the risk of the organization as with time and changes in healthcare regulations, such systems may not be able to meet the set standards.
Lack of vendor support:
This leaves the users in a very vulnerable position when vendors decide to pull out support for these legacy systems by ceasing to release updates or offer technical support.
Difficulties in data integration and sharing:
If legacy systems isolate patient data that fail to support a patient’s holistic care, then it is time to modernize.
Inability to support new healthcare initiatives or technologies:
Those that cannot interface with new technologies such as telemedicine applications or AI-based diagnostic devices can slow down an organization’s advancement.
Healthcare Legacy System Modernization Strategies
When modernizing legacy healthcare systems, organizations have several strategies to consider:
Replacing vs. supporting:
Evaluate whether to completely replace or continue supporting legacy systems. This decision should be based on factors such as cost, system criticality, and available alternatives. In some cases, a phased replacement approach might be most appropriate.
Cloud computing and migration options:
Thus, using cloud computing in healthcare technologies you improve the scalability and accessibility of your online learning resources. Solutions implemented in the cloud can be more elastic and thus can underline the necessity of less infrastructure. For instance, migration of a conventional HIS to a cloud-based environment can enhance the access to services and scale down the infrastructure at the facility.
Mobile re-platforming for legacy applications:
Modify specific existing systems for mobile to improve their usability. This can enhance user experience and enable advanced models of healthcare services provision. For instance, to access the old EHR systems, mobility can enhance the productivity of physicians and the quality of care on the patient’s side.
Leveraging AI and big data analysis:
Adopt analytics solutions to enhance the quality of decision-making. AI in the context of healthcare can improve diagnostic results and contribute to the development of individual treatment strategies. This could encompass live processing of new data on top of old IT systems to generate new intelligence.
Enabling APIs for improved interoperability:
The suggestion is that standard interfaces should be used to enhance the integration of the systems. This can help to avoid the scenario where a patient is transferring within different healthcare systems and his or her records do not go along with the patient. For instance, adopting HL7 FHIR APIs in legacy systems can be quite useful in enhancing communication between the system and the new-age healthcare applications.
Steps to Modernize Healthcare Legacy Systems
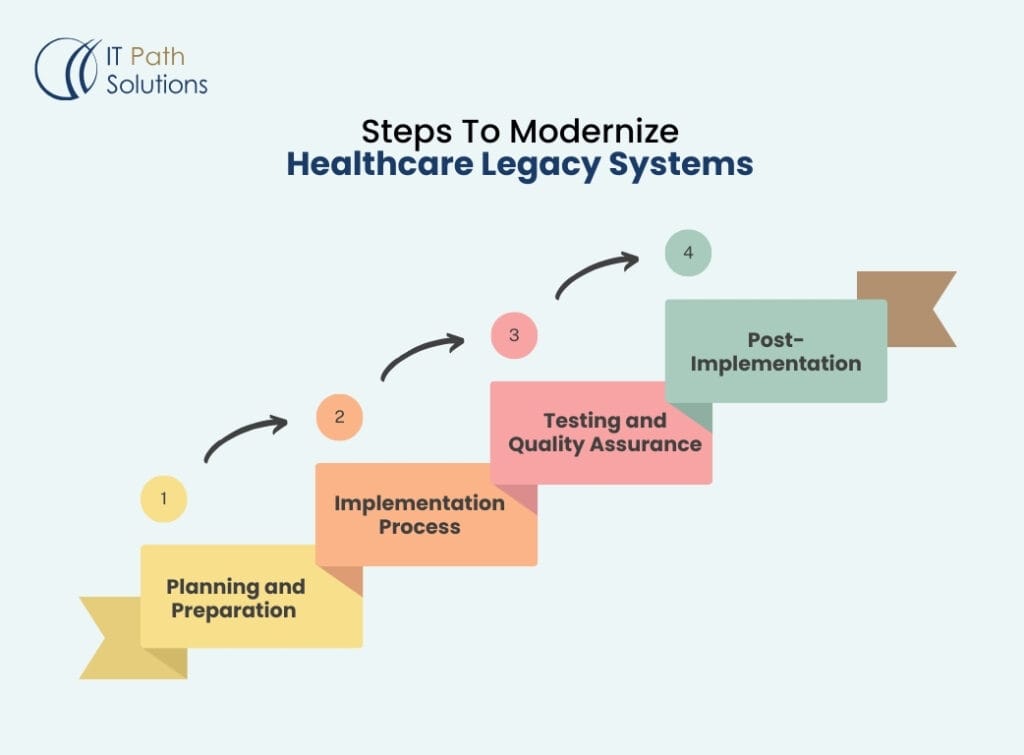
A. Planning and preparation
Conducting a thorough system evaluation:
Evaluate the current systems and their advantages and disadvantages. Such evaluation should capture performance, user satisfaction, and compliance with current models of health care. In essence, there is a need to identify which components of the legacy systems are relevant and which are obsolete.
Setting clear modernization goals:
The next step is to set clear goals for the modernization process to be completed in the company. These goals should reflect the organization’s strategic plan and mission when it comes to the delivery of patient care. These might be objectives relating to data availability, the strengthening of security features, or the creation of new care paradigms.
Choosing the right modernization approach:
Choose the right approach depending on the situation in the organization. This may be done in phases, involving the replacement of all the systems or some of them and the rest at another time. Look at issues like cost, the effect on operations, and the viability of the strategies in the long run.
B. Implementation process
Data migration strategies:
Organize and perform the migration of information from the old to the new platforms. This should be done in a way that maintains the data’s accuracy and has little impact on the organization’s current activities. It may include data cleaning, data conversion, and other validation processes.
Integration methods (middleware, API):
Enact measures that would enable the integration of communication between the systems. This may require HL7 Integration or any other standard healthcare application development interface for data sharing. Middleware solutions can play the role of interpreters between old and new environments, thus facilitating the transition.
Testing and quality assurance:
Thoroughly check new systems so that the quality and effectiveness are not compromised. This should comprise stress testing, user acceptance testing, and security auditing. There are two goals: focus on maintaining data consistency and on the program’s response time in different situations.
C. Post-implementation
Monitoring and optimization:
Monitor the performance of the system and where necessary, make improvements. This is where the need to conduct constant audits and get feedback from the users comes in to help in realizing the continuous improvement areas. Establish performance measurement systems as preventive measures to correct problems and enhance the operation of the system.
Staff training and change management:
Make staff ready and support them to go through the change process. It is important to note that adequate training and effective communication are critical when it comes to implementation. It may be useful to assign “super users” who will help educate others and be advocates of the new systems.
Overcoming Common Modernization Challenges
Modernizing legacy healthcare systems comes with its own set of challenges: Modernizing legacy healthcare systems comes with its own set of challenges:
Addressing interoperability issues:
The new systems must be able to integrate and interconnect with the existing environment. This may include such measures as maintaining a consistent format of data and communication protocols. It is wise to integrate organization-specific standards such as HL7 FHIR for improved data sharing.
Enhancing user interfaces for better engagement:
Design intuitive interfaces that enhance the user experience. Modern UIs can help minimize the number of steps employed in the use of an application or interface to complete a task while also minimizing the number of mistakes a user can make. Engage the end-users so that they can help define what the new interfaces should look like.
Strengthening security measures:
Introduce strict measures of protection for the various types of health information that exist. This includes a method of protection such as encryption, allowed or restricted user access, and routine security patches. One should also introduce multi-factor authentication and role-based access control to improve data security.
Breaking down data silos:
Facilitate seamless data sharing across different departments and systems. This can improve care coordination and support comprehensive patient management. Implement data governance policies to ensure consistent data management across the organization.
The Future of Healthcare IT: Trends and Innovations
As healthcare organizations move beyond legacy systems, several trends are shaping the future of medical technology: Below are several trends that define the future of medical technology as healthcare organizations are stepping out of the traditional systems:
Artificial Intelligence in healthcare:
Diagnostic and therapeutic support with the help of AI are advancing too which creates a great potential for the further development of individual approach in medicine. AI can also perform analysis on a large number of patients’ records and prescribe therapeutic measures that may go unnoticed by human clinicians.
Telemedicine systems:
Due to advanced technology, patients and consumers can access telemedicine and telerehabilitation, virtual consultations, and patients’ compliance and change in access to health services. Indeed telemedicine has been on the rise due to the COVID-19 outbreak and this will also continue in the future.
Blockchain for secure health data management:
This position offers a new chance to create a safe and decentralized means of sharing of health information. Blockchain can enhance the quality of data, increase the compatibility of the systems, and inform patients about their records.
Internet of Medical Things (IoMT):
Mobile health (mHealth), and telemedicine for continuous/ritual patient checkups are the greatest advancements in chronic disease and preventive care management. Whether it is a smart inhaler or a wearable ECG monitor, IoMT devices are generating data of tremendous value for patients.
5G technology for faster data transmission and improved connectivity: This is the next-generation network technology that will enhance the characteristics of telemedicine and provide healthcare solutions. 5G can enable surgeons to conduct operations remotely and transfer large medical files such as imaging files.
Conclusion
The process of healthcare IT system modernization is a challenging yet crucial task for healthcare organizations that desire better patient care, increased efficiency, and better competitiveness in today’s world. Legacy systems have inherent issues that can be a barrier to achieving more advanced, secure, and efficient technologies in healthcare; however, by utilizing proper modernization strategies, healthcare providers can overcome all these difficulties.
Transforming medical technology that has been practiced in the past to the advanced healthcare systems that are present in the world today needs a lot of planning, capital, and constant development. Nonetheless, the advantages of this shift such as better health quality, better business productivity, and better security of information overpowers the difficulties.
With the constant progress in healthcare, organizations that modernize their legacy systems will have an advantage in adapting to changes in care delivery models.
Additionally, utilizing innovative technologies can significantly impact the quality of care provided to patients.
Digital, data-driven, and connected healthcare is already here, and it starts with the transformation of the industry’s core infrastructure.
FAQs
1: What is a healthcare legacy system?
A healthcare legacy system is outdated software, technology, or a process that is no longer supported, updated, or maintained due to newer, superior technology. These systems often remain in use because they are critical to operations but can pose security and efficiency risks.
2: Why do healthcare organizations continue using legacy systems?
Healthcare organizations may keep legacy systems because they are deeply integrated into daily operations, replacing them can be costly, and newer alternatives may not seamlessly support existing workflows or data exchanges.
3: What security risks do legacy systems pose to healthcare organizations?
Legacy systems often lack vendor support, security updates, and patches, making them vulnerable to cyberattacks, data breaches, and compliance violations. This increases the risk of ransomware attacks and HIPAA non-compliance.
4: How common are legacy systems in healthcare?
According to a 2021 HIMSS survey, 73% of healthcare providers still rely on legacy information systems. Many organizations use multiple outdated applications, increasing cybersecurity and operational risks.
5: What steps can healthcare organizations take to manage legacy system risks?
Organizations should conduct regular security audits, implement cybersecurity training, ensure compatibility with new technologies, eliminate data silos, and assess performance and maintenance costs. When possible, transitioning to modern systems should be prioritized to enhance security and efficiency.
Keyur Patel
Co-Founder
Keyur Patel is the director at IT Path Solutions, where he helps businesses develop scalable applications. With his extensive experience and visionary approach, he leads the team to create futuristic solutions. Keyur Patel has exceptional leadership skills and technical expertise in Node.js, .Net, React.js, AI/ML, and PHP frameworks. His dedication to driving digital transformation makes him an invaluable asset to the company.
Get in Touch
Search
Blog Categories

